Even though my research has focused on the topic of multimorbidity for the majority of the past two years, I did not imagine it would throw me as hard as it did when it came close to home.A family member of mine has become one of the many unfortunate examples of today’s fragmented health and social care system. Besides chronic kidney disease, he does not suffer from any of the common or typical chronic health conditions such as diabetes, obesity, lung disease or dementia. Currently he receives care from several professionals; each and every one of them being highly qualified, specialised and competent in their discipline. The nephrologist and his assistants look after his kidneys, the cardiologists and his team keep an eye on his heart, the dermatologist and his assistants are making sure they catch changes in the skin early, the oncological team itself comprises several different sub specialisms based on the different locations of malign cells (e.g., stomach, blood, etc.), a neurologist is looking out for potentially returning attacks in the brain, the dietician is concerned with his nutrition, etc. Long story short, the man is surrounded by professors, specialists in training and doctors!
Besides these professionals, located in the hospital, he also receives daily care from nurses who help him getting dressed and washed in the morning. His wife takes care of his tube feeding on a day to day basis, his daughter and son in law support the practical side of things (e.g. transportation to and from the hospital), his neighbour helps his wife to clean the house, etc. One would say he is in good hands (which he sure is), but he is also in many hands…
The biggest room in the world is the room for improvement – [unknown]
Normally I have to accept the fact that I (at most) can only provide some advice or suggestions from a distance. However, during my Christmas break, I was able to spend some time closer to him and the rest of my family. It was exactly during this break that it hit me how many people there are involved in his care – and more so, how little they know about one another.
Even though each and every actor involved does his/her job with precision and devotion, they barely know what is going on with the patient outside of their ‘disease box’. It is as if they are wearing blinders and in a way they are forced to do so. The need for highly specialised personnel has made it impossible for care providers to be up to date or informed about all the other disciplines. This is not necessarily a bad thing and there might be some truth in the saying ‘every man to his own trade’. Maybe they do not even need to know much about the other boxes that this patient ticks. I also do appreciate that the workload in health and social care is incredibly high! I acknowledge that each discipline has his concerns, series of protocols and/or rules of thumb. A lot of other factors and influences further contribute to maintaining this often ‘fragmented’ way of care delivery. During my internships in nursing, I got a daily glimpse of all this, so I do empathise with the hard work these professionals display on a daily basis.
It is exactly because I empathise with this group of providers and carers that all of this seems even more important. It is because I empathise with them, that I want nothing more than seeing them reach their goal! Regardless of their discipline, title, function, task in the care network,… they all have one goal in common: helping this man!
The single biggest problem to communication is the illusion that it has taken place – [George Bernard Shaw]
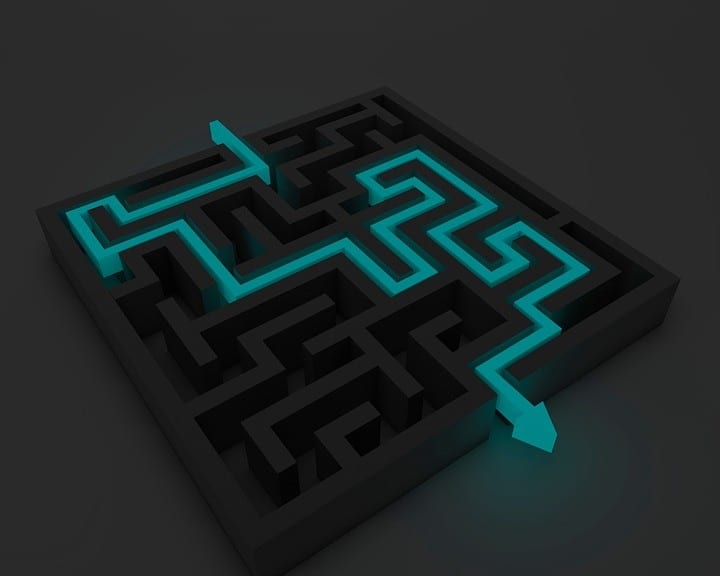
Each individual is putting in a big chunk of his/her time, resources, effort, knowledge, etc. towards helping him. However, there seems to be one big obstacle in reaching this goal: communication (or the lack of it). He has a complex maze to navigate in order to receive the ‘help’ he and his wife should get. The difficulty in navigation becomes even more burdensome if the different actors involved in his care barely communicate with one another. A couple years ago for instance the nephrologist told him not to take diuretics (because of his kidney condition), however he was prescribed that exact medicine when being admitted for a non-kidney related issue. Obviously this left him and his wife confused and insecure. Around the same time, after weeks and months of communicating to the dietician and oncologists that he was not drinking and/or eating, we rushed him to hospital with signs of severe dehydration. After his organs began to fail, they decided to provide him with tube feeding for about a year! More recently, the same story developed and yet again it took us rushing the man to the hospital with dehydration symptoms before anyone would really do something about it. Tests have been repeated because those ordering the test did not know it had already been done or was scheduled for another time. Medication has been added to the already extensive list, some of which interfered with what was already on that list, others were merely given to treat the side effects of an interaction of prescribed medicine, etc.
On top of the sometimes lack of information/communication, there are moments during which communication does happen, but in rather vague terms. After finishing his course of chemotherapy for instance, the oncologist said that “the chemo did its job”. However, no one knew what the set “job” was for the chemo to do. So, this could mean anything from ‘curing’ to ‘stabilising’ or ‘shrinking’. If I would not have contacted his GP to find out more about his current condition, we would not have known which type and/or stage of cancer he was diagnosed with. If my background in nursing would, for example, not have provided me with some insights into what ‘aids’ there are available (e.g. personal alarms), he and his wife would not know of their existence. But, as much as I like to help them, truth be told, this is not my job. Not only am not with my family 24/7 as I live abroad, I also need to trust the providers involved to ‘take care of him’ and know that they are far more educated and trained to do so than I am.
Real change requires a desire to change – [Gabrielle Bernstein]
There are endless examples and stories, both within my family as well as beyond, to illustrate communication issues in health and social care. As I said before, all the providers involved, are doing the best they can! If our society is to continue and uphold the highly specialised care environment we see today, some sort of ‘integration’ needs to be put in place somewhere, sooner rather than later. Whether or not this might be the task of a GP, is a story in itself, but the need for integration is increasing every day! Not only for the patients in question, also for all who are involved in care delivery and even our wider society.
Unnecessary repetition of tests, medications that interfere with each other, etc. do not immediately scream efficiency. If anything, it costs our society a lot of money and patients and their family a lot of hassle. Moreover, poor communication and lack of integrated services is ‘dangerous’. Each and every health and social care system has its advantages and disadvantages, but globally, all of them are facing these issues of communication and integration. We can be proud of the evolutions and developments that have happened and continue to happen in medicine, health and social care! They have made it possible for people to live longer, but we should not stop there. Our society will bear the cost if ‘living longer’ is all we establish! People need to live longer better and one step in that direction is by bridging the gaps that currently exist across health and social care systems around the world.